About Macular Degeneration
Age-related macular degeneration (AMD) is the most common cause of severe vision loss in patients over 65. This condition involves a breakdown of the macula, the central part of the retina responsible for detailed visual tasks such as reading and driving.
What Causes Macular Degeneration?
Many older people develop macular degeneration as part of the body’s natural aging process. Our eyes and retina develop signs of aging just as our skin shows signs of the aging process. Exactly why it develops is not known, and there is no cure available.
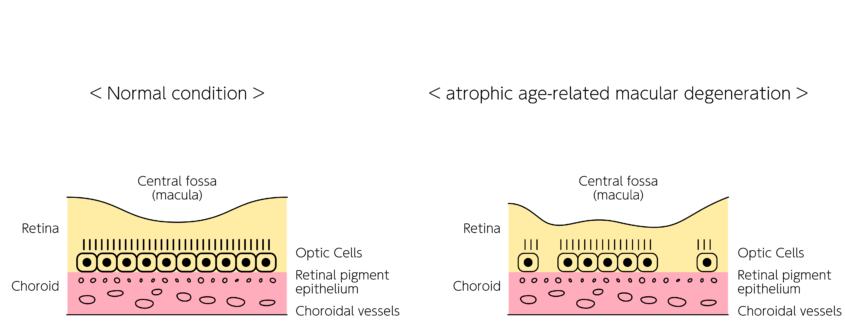
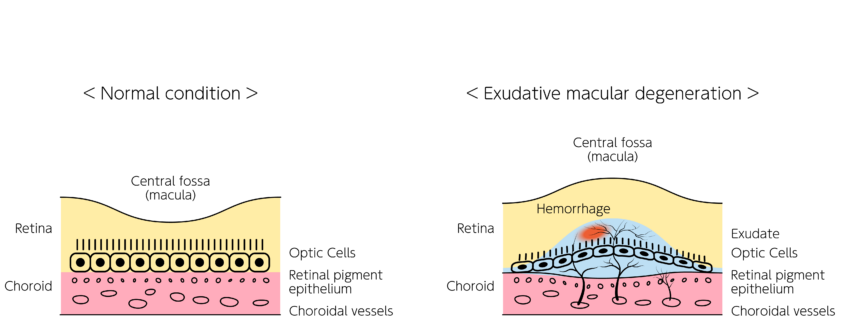
Two Types Of Macular Degeneration
Most people with AMD have the “dry” type. It is caused by the aging and thinning of the tissues of the macula. Vision loss is usually gradual. Deposits under the retina called drusen are a common feature of AMD. Drusen alone usually do not cause vision loss, but when they increase in size or number, this generally indicates an increased risk of developing advanced “wet” AMD. The dry type can progress into the “wet” type, and this accounts for about 10 percent of all patients with AMD. Wet AMD results when abnormal blood vessels develop underneath the retina at the back of the eye. These new blood vessels are fragile and often leak fluid or blood, causing blurry central vision. In contrast with dry AMD, patients with wet AMD often, but not always, experience sudden and severe vision loss.
Macular Degeneration Symptoms
When the macula does not function correctly, your central vision can be affected by blurriness, dark areas or distortion. The degree of damage to the macula can vary from patient to patient and the symptoms can range from mild to severe. In the vast majority of cases, AMD does not automatically progress to blindness. Although AMD reduces vision in the central part of the retina, it usually does not affect the eye’s peripheral, or side, vision. Even patients with advanced macular disease tend to retain excellent peripheral vision.
Diagnosis and Tests for Macular Degeneration
During your initial visit for macular degeneration, you will have a detailed examination of your eyes after your pupils are dilated. Sometimes it is difficult to distinguish between dry and wet AMD. Thus, our physicians may recommend a variety of clinical tests in order to make an accurate diagnosis. These tests may include fluorescein angiography (FA) and optical coherence tomography (OCT). FA involves the injection of a small amount of vegetable-based dye through a patient’s peripheral vein, usually the arm or hand. The dye is not the same contrast dye used for cat scans (CT), and thus, it is generally safe even for patients with abnormal kidney function. After the dye is injected, an ophthalmic photographer will take a series of time-dependent photographs as the dye circulates through the blood vessels in your retina. The dye lights up areas of abnormal and leaky blood vessels. Not only is this useful in determining the extent and progression of the disease, but it also helps when targeting specific treatment areas, comparing disease progression, and efficacy of treatment.
OCT is a non-invasive, quick photograph that uses light rays to measure the thickness of the retina. OCT provides a detailed, high magnified, cross-section view of the retina on a microscopic level. It can often reveal tiny areas of leakage not readily apparent during an exam. An OCT photograph is not an x-ray and is not harmful to your eyes.
Early detection of macular degeneration is important and often results in better visual prognosis. As a result, every patient diagnosed with macular degeneration should establish a daily routine for monitoring their own vision. This is reliably performed with an Amsler grid, a simple paper with straight horizontal and vertical lines similar to graph paper. We are happy to provide you with an Amsler grid at no cost; simply ask one of our nurses. New “waviness” or “broken/missing lines” on the Amsler grid can be a warning sign of subtle progression of your AMD. Should you or a family member notice new changes on the grid, contact us promptly.
If you are at high risk for developing wet AMD, you can now take a proactive approach to your eye health.
Frequent monitoring with the ForeseeHome™ AMD Monitoring Program provides a safety net for monitoring changes in your vision between office visits, allowing your doctor to detect and diagnose wet AMD at its earliest stage.
Macular Degeneration Treatments
Although the exact causes of AMD are not fully understood, antioxidant vitamins and zinc may reduce the risk of progression of AMD in some people. A large scientific study found that people at risk for developing advanced stages of AMD lowered their risk by about 25 percent when treated with a high-dose combination of vitamin C, vitamin E, zinc, and beta carotene. Not everyone may benefit from using these supplements, especially those patients with either no AMD or very early AMD. Patients who smoke are encouraged to use a vitamin formulation without beta carotene, as this high dose has been suggested to increase the risk of lung cancer in patients who smoke. Ask your doctor if you should consider vitamin supplementation.
Avastin and Lucentis are the first medicines that have actually improved vision for many patients with wet AMD. These medications are injected into the eye and help to block certain growth factors that cause abnormal blood vessels to “leak” in wet AMD. While the thought of an injection in the eye might cause many people to cringe, in our experience, there is little or no discomfort and the spectacular visual gains far outweigh any fears.
Although we have made significant progress in the battle against AMD, we still do not have a treatment that can restore vision to normal. Despite advanced medical therapy, many people with macular degeneration still experience some vision loss. The physicians at Retinal Consultants are dedicated to providing the latest technology available to treat AMD. We are actively involved in multiple clinical research trials in hopes of finding the next “cure.” Ask your doctor if you may be a candidate for one of our clinical research trials.
Diagnostics with ForeseeHome
There is currently no cure or treatment for dry AMD but there are steps you can take to reduce your risk of developing wet AMD. These include healthy lifestyle choices, like not smoking, and taking AREDS2 vitamins daily if recommended by your doctor. It’s also important to monitor your eyes with at-home testing between office visits. There is advanced home monitoring technology available that is sensitive to changes in AMD. The ForeseeHome® AMD Monitoring Program is an easy-to-use early warning system for your eyes that can catch the progression from dry to wet AMD as soon as it happens, which lets your doctor step in sooner and determine the appropriate course of action. People preserved more of their vision when wet AMD was detected using ForeseeHome between office visits, in addition to your doctor’s standard of care. ForeseeHome is FDA-cleared and covered by Medicare.

Diagnostics for AMD
FAQs
What are risk factors for Age- Related Macular Degeneration (AMD)?
Macular degeneration primarily affects older Caucasians, although it has been reported in younger individuals and multiple races. Cigarette smoking, high blood pressure, and a positive family history of AMD may predispose you to developing AMD. Although there is currently no way to definitively predict who will or will not develop AMD, those with affected relatives are at high risk. As a result, adult relatives of patients with AMD should schedule an appointment with a retinal specialist and undergo a baseline evaluation. Your doctor can then tell discuss your risk of developing the advanced form of AMD.
Can you prevent Age- Related Macular Degeneration (AMD)?
No, many older adults will develop AMD as part of the natural aging process. Frequent eye exams are a good way to screen for and monitor the progression of conditions like AMD.
Can Age- Related Macular Degeneration (AMD) be cured?
No, there is not currently a cure for AMD, but clinical trials and advances in technology are being discovered for new way to treat and manage the condition.
Hear what patients are saying
Conditions We Treat
Our ophthalmologists are experienced in diagnosing and treating many retinal conditions.
![iStock-1391156780 [Converted]](https://www.retinalconsultantsaz.com/wp-content/uploads/2023/12/iStock-1391156780-Converted.png)